Eye Conditions Treated
Dr Nazari is a specialist ophthalmologist with extensive expertise in doing complex cataract surgeries and managing medical retina conditions.
He has performed thousands of cataract surgeries with a focus on refractive outcome of surgeries and using latest sophisticated intraocular lenses.
Below is the information about the clinics services.
If you have any further questions please contact us.
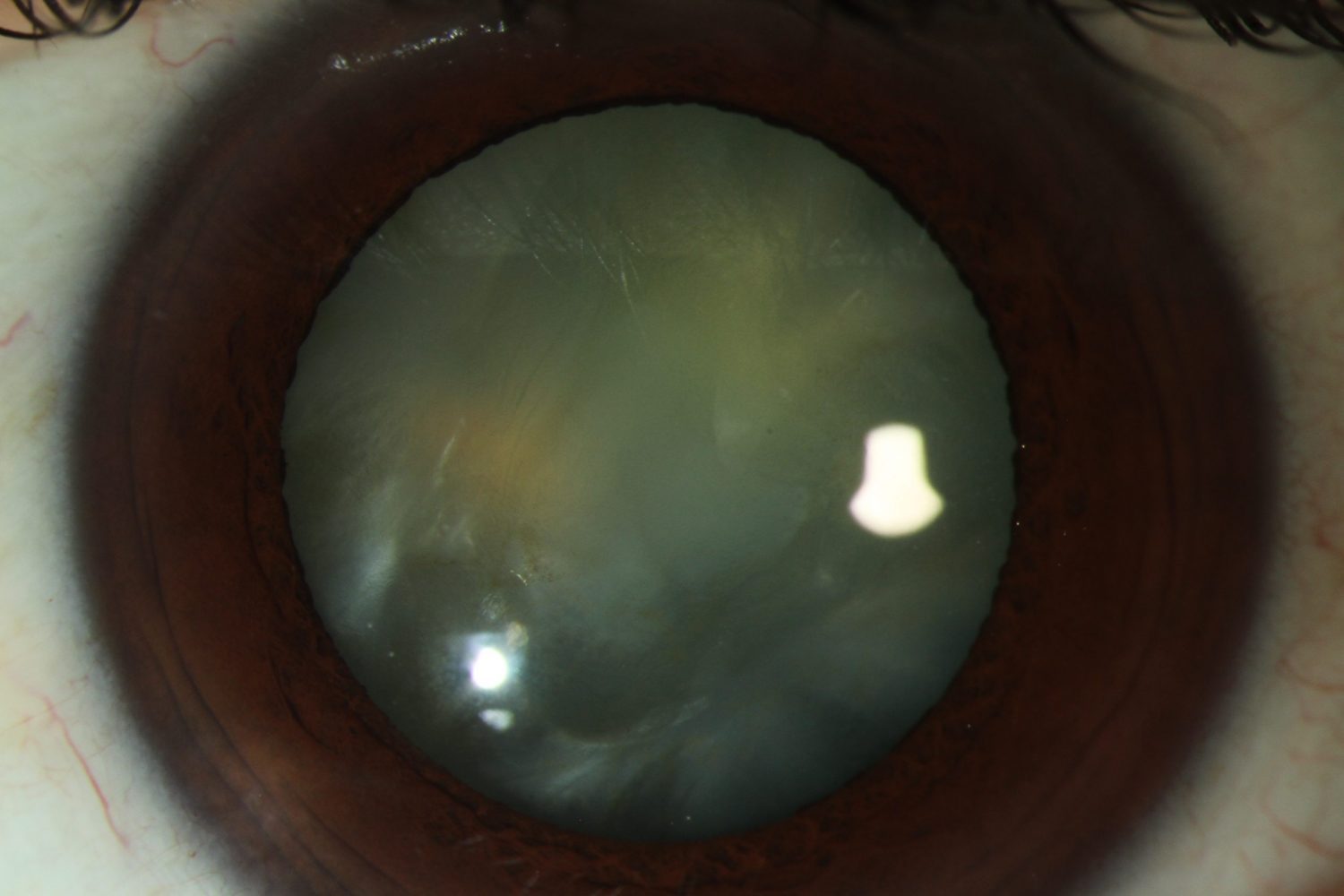
Cataract
Introduction
Cataract is when the clear natural lens in your eyes become cloudy. Most cataracts develop slowly and initially they may not interfere with your vision. When the condition deteriorates you may feel seeing the world through a frosted or opaque window.
Symptoms
- Blurred or foggy vision
- Increasing difficulty with vision at night with glare and “halos” around lights
- Frequent changes in eyeglass or contact lens prescription
- Fading or yellowing of colours
- Double vision through one eye

Causes
In most of cases cataract is secondary to ageing and changes happen in protein content of the natural lens. Other less common causes of cataract include trauma to the eye, long term use of steroid medications and eye surgery.
Treatment
Currently there is no medical treatment for cataract and the only way to improve the vision is doing a cataract surgery. The decision on doing a surgery depends on the extent of visual impairment caused by cataract and the effect of that on your lifestyle.
Before Surgery
A measurement will be done in the office to calculate the power of the intraocular lens (IOL) used during surgery. The choices for IOLs to correct your eye sight will also be discussed with you, along with all other details about surgery and the risks and benefits of doing such a surgery. We also ask about all your medical history, the medicines you take and your allergies.
The Day of Surgery
You will be asked to avoid eating solid foods for 6 hours and clear fluids for 2 hours before surgery.
Cataract surgery is generally done as a day procedure, which means you don't need to stay in the hospital overnight. It's a very safe surgery with a high success rate and very low risk of complications like infection, bleeding and severe inflammation.
- Your eye will be numbed using either an injection around that or numbing eye drops
- You will also be sedated to have maximum of comfort
- Your surgeon then will remove the cataract using sophisticated instruments and will put an Intraocular Lens (IOL)
- Usually there is no need to put stitches and the small wounds created during the surgery are self sealed.
- The whole surgery usually lasts around 15-20 min.
Care after Cataract Surgery
You will be discharged from the hospital with a pad or clear plastic shield on the operated eye. You can remove the pad the day after surgery but you need to keep the plastic shield on the eye most of the time during the first week after surgery.
It is normal to have some symptoms of grittiness, watery eye, mild discomfort, blurry vision and red eye but these side effects usually revolve in a few days. The full recovery after cataract surgery may take 4 to 6 weeks.
When to Seek Help
If you have an increasing pain or eye redness or your vision is deteriorating, you need to call your surgeon immediately or see an ophthalmologist in Emergency Department at The Royal Victorian Eye and Ear Hospital.
Dos and Don'ts
For the first weeks after surgery:
Do
- Your normal daily activities including watching TV, reading on computer and going for a walk outside
- Use the drops prescribed to you after the surgery
- Have your eye shield on the operated eye, especially at night, for 1 week
- Take a quick shower while having the shield on the eye
Don'ts
- Rub the eye
- Swim for 4 to 6 weeks
- Do any strenuous activities
- Wear make up for 4 weeks
- Drive until confirm it with your surgeon
Glaucoma
INtroduction
Glaucoma is a group of diseases which cause visual loss by damaging the optic nerve. The loss of sight initially starts from peripheral field of vision and as a result most of patients don't notice that in early stages.
In most of patients, the pressure in the eye is higher than normal and it gradually damages the optic nerve. Some people with high pressure in the eye never get glaucoma and some patients who are suffering from glaucoma have normal pressure. This confirms that several factors contribute in causing glaucoma and in progression of the disease.
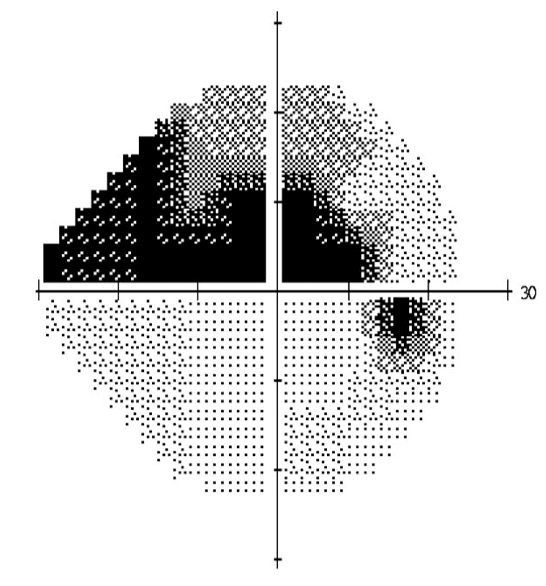
Normal Vision

Glaucoma
For further information about glaucoma click the below image:
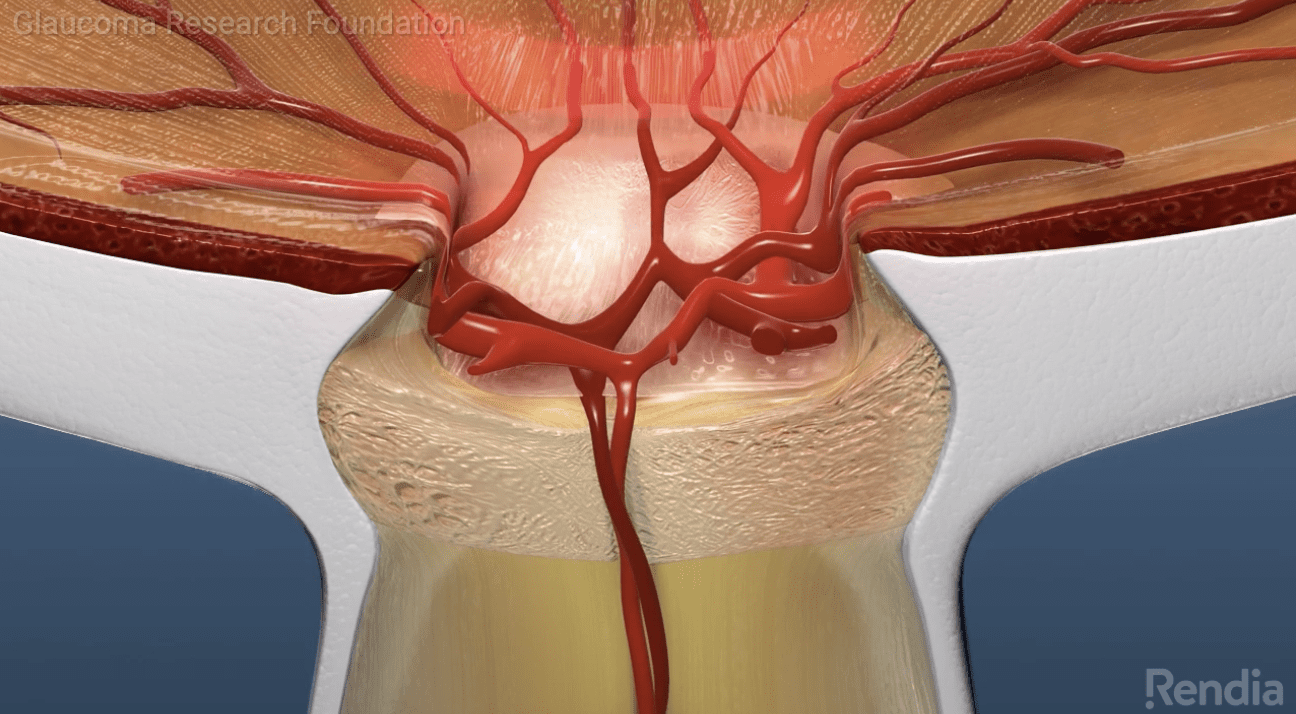
Treatment for Glaucoma
Medications
Drops are the most common form of treatment for Glaucoma, but sometimes tablets or intravenous medications may be needed to control the pressure in the eye.
Laser Peripheral Iridotomy
This a laser done for patients who are differing from angle closure glaucoma or at risk of that.
Selective Laser Trabeculoplasty
Selective Laser Trabeculoplasty (SLT) is done in patients with open angle glaucoma. There is increasing evidence supporting using SLT as an alternative to eye drops for initial treatment of glaucoma. It is also an option when the patient faces side effects of using drops or cannot use them.
Surgery
A surgery may become necessary if conservative treatments like drops and laser fail to stop disease progression. This include incisional surgeries like Trabeculectomy and using shunt tubes. The aim in all of these surgeries is to safely open a pathway through the Wall of the eye to outside to drain the fluid from the eye.
Minimally Invasive Glaucoma Surgery (MIGS)
Minimally Invasive Glaucoma Surgeries are a group of surgeries which use micro implants to drain the fluid from the eye. They reduce the risk of having complications compared to traditional incisional surgeries and have shown promising results.
iStent
is one of the most common MIGS surgeries done in the world. It is usually implanted during cataract surgery and considering its very low risk of complications is a good option for patients suffering from glaucoma.
Diabetic Retinopathy
Overview
Diabetic retinopathy is a damage of the sensory layer in the back of the eye (retina) secondary to the damage to small vessels because of longstanding poorly controlled diabetes.
Symptoms
Although Diabetic Retinopathy is asymptomatic at the beginning, it may eventually cause any of the following symptoms:
- Blurred vision
- Dark spaces in the field of vision (scotoma)
- Fluctuations of vision
- Floaters
- Loss of vision
Normal Vision

Diabetic Retinopathy
Early (Non-Proliferative) Diabetic Retinopathy
In Non-Proliferative Diabetic Retinopathy (NPDR) the walls of small vessels in the retina weaken and leak lipid material and fluid to the surrounding tissue. This causes swelling of retinal tissue and when it happens in the centre of macula, it can cause vision loss and needs treatment. The nerve fibre layer of retina may also swell (Cutton Wool Spots) and multiple bleeding spots may happen in the retina. In the more severe form of the disease, large vessels of the retina may become dilated and irregular.
Advanced (Proliferative) Diabetic Retinopathy
In Proliferative diabetic Retinopathy (PDR), small new vessels grow in the retina which may bleed into the clear jelly-like material fills the eye (vitreous) and cause a severe visual loss. Without treatment, these new vessels eventually may cause glaucoma or scar tissue resulting in retinal detachment and may lead to blindness.
Prevention
It is not always possible to prevent Diabetic Retinopathy, however with regular eye examination, good control of blood sugar and cholesterol level and hypertension the risk of developing Diabetic Retinopathy decreases significantly. If you smoke, you definitely need to discuss with your doctor the options to quit.
Diagnosis
Diabetic Retinopathy is best diagnosed with an eye exam when the pupil is dilated. For this exam drops are put in your eye to make the pupil wider, but this will cause a blurred near vision for about 6 hour and you will not be able to derive after the exam for this period. Your ophthalmologist will then examine your retina for signs of Diabetic Retinopathy and check the pressure of your eyes to exclude glaucoma.
Optical Coherence Tomography (OCT)
Your ophthalmologist may request an OCT for further assessment of your retina. This is a special image which shows different layers of retina and helps to exclude swelling of retina.
Treatment
While Non-Proliferative Diabetic Retinopathy only needs better control of diabetes, hypertension and hypercholestrolemia, for Proliferative Diabetic Retinopathy you need an intervention by your ophthalmologist. This can be injecting of a medicine into your eye or doing retina laser treatment. In very advanced form of the disease you may need a vitrectomy surgery.
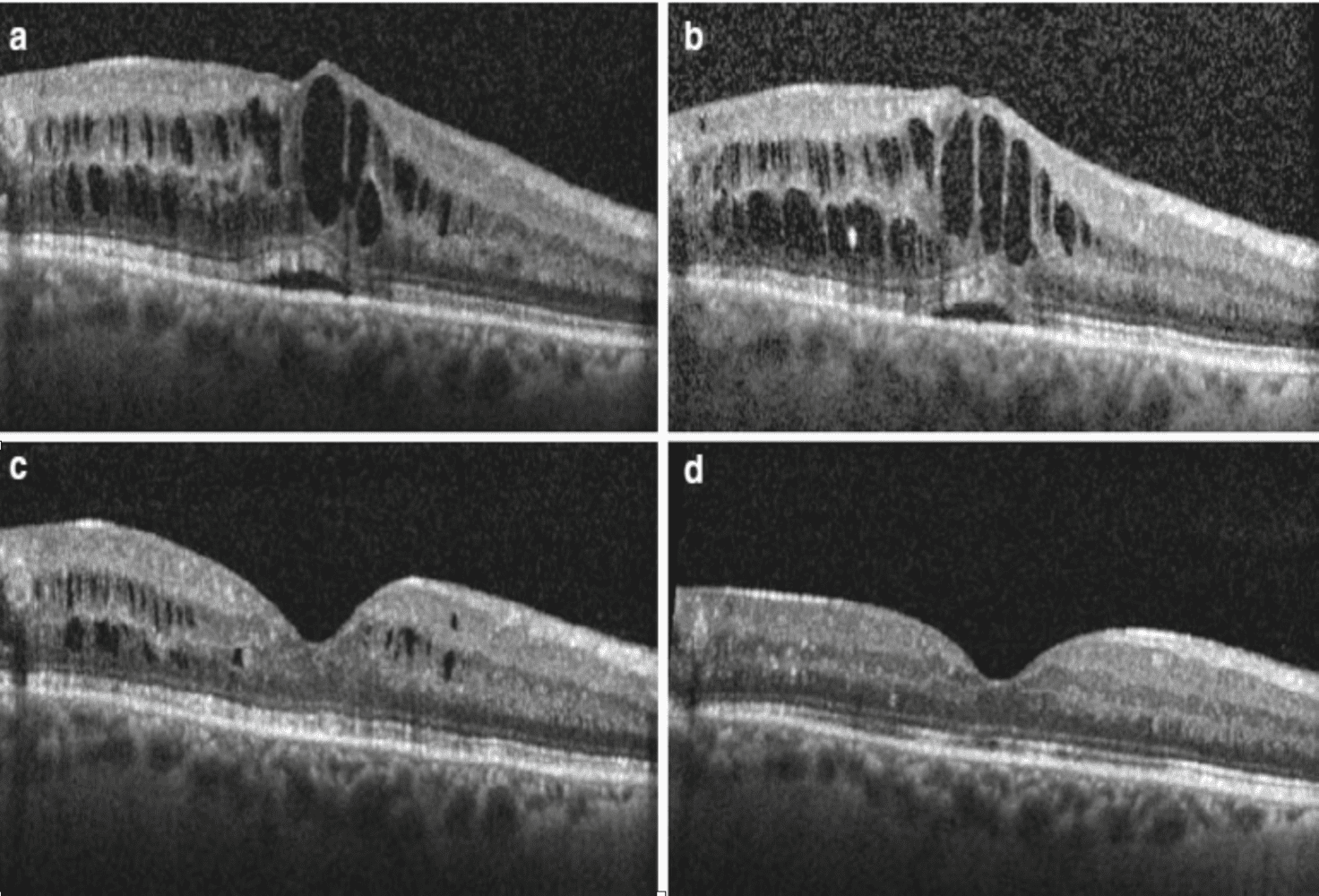
Effect of injection medicine into the eye on Diabetic Macular Oedema
For further information about glaucoma click the below image:
Age Related Macular Degeneration (AMD)
Overview
Macula is the central part of the sensory layer in the back of the eye (retina). In Age Related Macular Degeneration (AMD) this area becomes affected and this causes a deterioration of central vision and problems with reading, detecting faces and any other activities that require detailed vision.
Stages of Macular Degeneration
Early Stage
This stage usually happens in patients older than 50 and caused by gradual built up of waste material (Drusen) beneath the retina. Most of patients at this stage don't have any symptoms. There is no treatment available for this condition, however having a healthy diet, avoiding smoking and a good control of systemic conditions like hypertension decreases the risk of progression of the disease to more advanced forms.
Late Stage
At this stage central vision become impaired and can be subdivided to Dry type (Atrophic) or Wet type
(Neovascular) Macular Degeneration.
Dry Type: Atrophy (loss) of sensitive nerves in the macula happens leading to a gradual loss of central vision. There is no proven treatment available for this condition.
Wet Type: Abnormal fragile vessels grow beneath and in the retina which leak fluid and blood. It usually causes a rapid decrease in central vision.
Normal Vision

Advance AMD
The main treatment for advanced Wet AMD is injecting a medicine directly into the eye. It is done in the clinic using a sterile technique and gives you a good chance of maintaining or improving your vision.
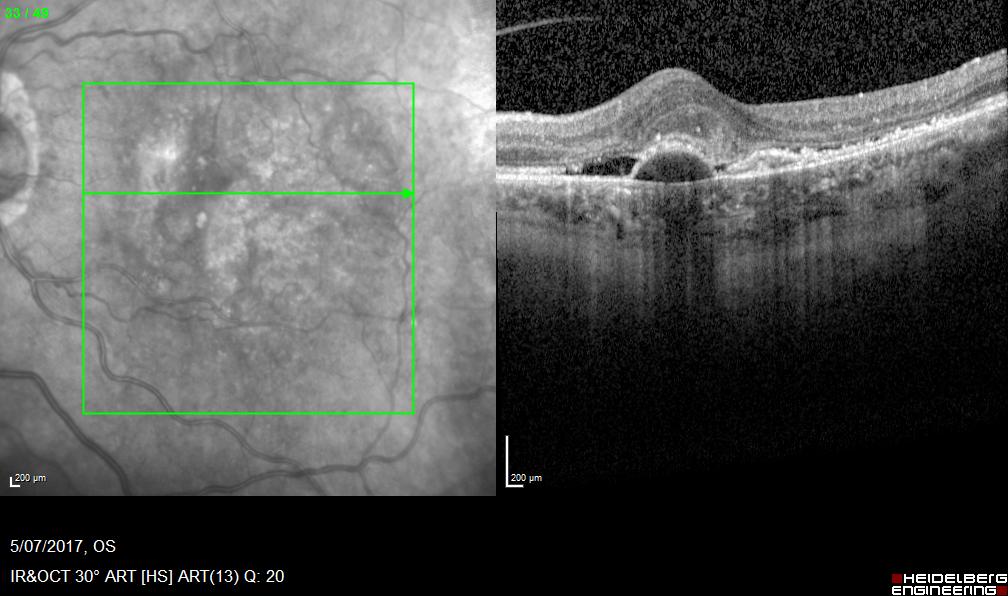
Wet AMD before treatment
Visual acuity 6/24
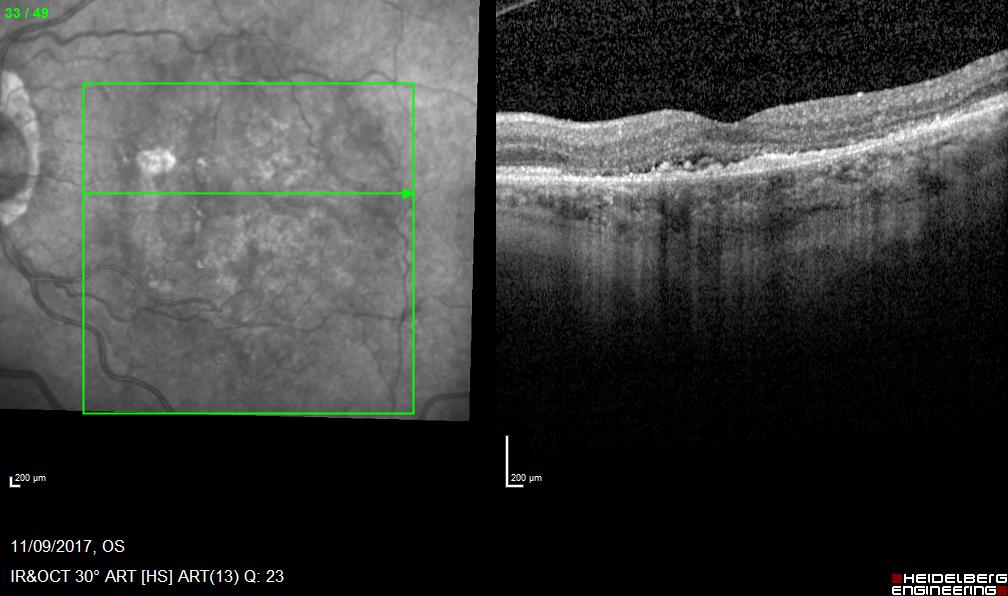
Wet AMD after treatment
Visual acuity 6/9